Culturally Competent mental health services
Content Warning: This post DISCUSSES mental illness (depression, suicide) and systemic racism
So... What's Cultural Competence?
Cultural competence is the ability to address the needs of individuals through an intersectional lens that recognizes the social locations and dimensions that influence our unique identities and experiences.
Culturally competent care involves using equity and inclusivity to guide treatment so that services are supportive to all marginalized folks - without perpetuating harm and reinforcing existing barriers
Quick note! A ton of different language is used to talk about culturally competent services, and no term is perfect. Whether it be therapists employing 'cultural humility', or services being 'culturally responsive', every term has its purpose. No matter what word you use, it's about accepting the life experiences and perspectives of others. Judgement free.
Who is Left Out?
Canada is facing a disastrous mental health crisis—one that most disproportionately affects BIPOC and marginalized communities.
A survey of people who experienced a major depressive episode found that BIPOC communities were far less likely to seek help.
Sharing common ground allows us to build meaningful trust with each other; 60% of Black Canadians reported that they would be more willing to speak to a mental health professional if they were Black.
It's no secret that the pandemic has left many of us in the Bad Place, however, BIPOC report experiencing up to 2X worse self-rated health than white people.
Culturally Competent Care
Colonial and racist legacies have worsened the fear of judgment and isolation for generations, exacerbating mental health conditions. Couple that with the ancestral and intergenerational trauma and cultural nuances, and internalized cultural racism, sexism, etc., that so many of us knowingly and unknowingly carry with us.
Take it from us; language matters. Not being able to clearly identify and begin to unpack the nature of systemic oppression and your unique ancestral and culturally rooted experiences is a disservice to your healing. Without culturally competent services and training, even the most well-intentioned mental health professionals (even if they are racialized) can end up framing your care through a Western lens—steeped in the same racism, ethnocentrism, ableism etc. that our systems are.
“I mean, who’s best to say how something hurts and why something hurts than the people who are experiencing it — not random doctors who think they’re trained in cultural competence.”
Systemic Barriers
It can be really scary asking for help, not to mention that stigma, language barriers, fear/distrust of services, and previous negative experiences with the healthcare system make it *that* much harder for marginalized folk to feel safe seeking care. No one wants to be discriminated against by the very person they went to help for.
Current treatment plans emphasize medication and individual behaviour change. These can be incredibly isolating and damaging to those who come from collectivist cultures. This approach also often fails to hold systems of oppression accountable and discourages collective healing related to intergenerational trauma.
Not to mention that most assessment tools and services are created by and for a very specific subset of the population (read: white, straight, cis, middle/upper class from the Global North) while ignoring the perspectives and experiences of everyone else. Our lived experiences and accompanying health issues are often not accurately captured in the DSM-5.
Life-Saving Care
“[It’s about] ... recognizing that wellness for us as Indigenous peoples isn’t just based on a western medical model. It’s our families. It’s our communities. It’s our bodies. It’s how we’re feeling emotionally, physically, mentally and spiritually.”
Access to culturally competent mental health services can be life-saving for marginalized folk who face endless barriers to care. Speaking to a professional that can understand and relate to your experiences creates a space of trust and empathy. Responsive services can also help to unpack (and even end) cycles of generational trauma, reduce the deep sense of isolation that BIPOC and 2SLGBTQIA+ communities often face, and reconnect individuals to their culture. These services see the person as a whole, not just a diagnosis.
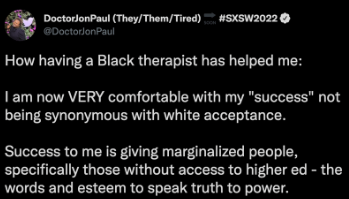
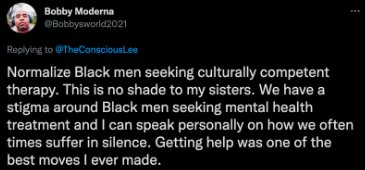
Success Stories
Hear about the magic culturally competent care can do:
What Can You Do?
Educate yourself
Learn more about the barriers that BIPOC, recent immigrants, refugees, and 2SLGBTQIA+ communities face that impact their access to quality health care. Check out our other mental health posts to learn more. Listen to and uplift marginalized voices.
Initiate and de-stigmatize discussions around mental health within your communities
If we don't keep talking openly and honestly about mental health, restrictive systems and other barriers to care will continue to go unchecked. Facilitate change in your network by speaking up and speaking out! #MentalHealthAwareness
Donate to initiatives that support marginalized folk in obtaining culturally competent care
Consider supporting these groups that uplift those who are making a difference: Black Healing Fund, Asian Mental Health Collective, Across Boundaries, Anishnawbe Health Toronto
What Canada Must Do
Canada loves to brag about being a mosaic of different people, cultures and ethnicities, but our current healthcare system does not reflect this diversity. There is an urgent need for more diverse staff and comprehensive cultural formulation and diversity training for providers.
Mental health is part of overall health, so it should be publically funded (aka free via our taxes), along with visits to health care providers, hospital visits and (scream it with us) prescription drugs.
Whether it's because of transport, service availability, or ridiculous wait times (ranging from 25 to 260 days!), accessibility is a major barrier to care. Telemental health care (which brings the professional to your screen) can help more people access the care they need.
Ultimately, more preventative work needs to be done to address inequities and provide meaningful support. Fund marginalized communities. Provide affordable housing for people experiencing homelessness. #DefundThePolice.
Mental Health Resources
If you or someone you know is in crisis, visit an emergency department or call 911
If you or someone you know needs support:
Canada Suicide Prevention Service: 833-456-4566
Multicultural Women Against Rape: 416-597-8808
National Indian Residential Schools Crisis Line: 866-925-4419
Elbow River Healing Lodge - Alberta: 403-955-6600
Althea Therapy: altheatherapy.com
Black Youth Helpline: blackyouth.ca
Asian Mental Health Collective: asianmhc.org
South Asian Therapists: southasiantherapists.org
Take some time to get to know the local resources in your region and keep a list of resources on-hand!
Sources: Canadian Mental Health Association. Mental Health Commission of Canada, CTV. StatsCanada, CAMH, Ontario Human Rights Commission, Calgary Journal, Twitter, The Star